HEALTH
Speech Therapy Taxonomy Code: Start Using the Right One Today
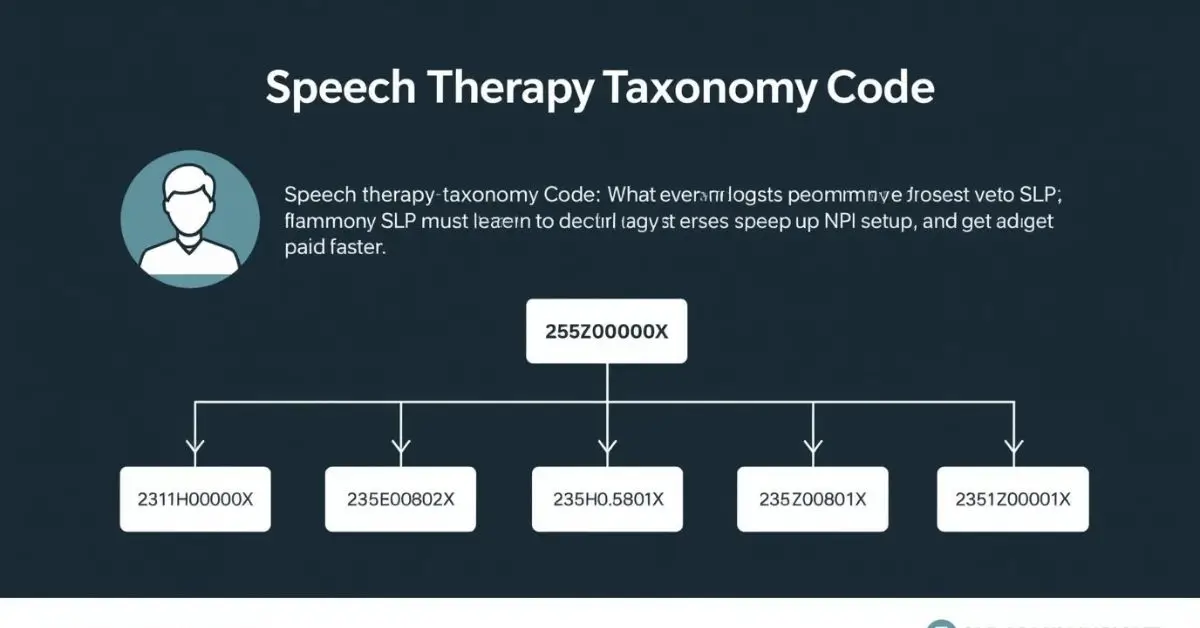
Are you struggling to figure out which speech therapy taxonomy code to use for billing or NPI registration? Whether you’re a healthcare provider, billing specialist, software vendor, or clinic administrator, getting this code wrong can delay insurance payments and cause compliance issues.
Ever wonder why that is? Taxonomy codes are like a digital handshake they tell insurers exactly what your specialty is. But if you’re an SLP, the system can be confusing. This guide will break it all down in plain English so you can avoid billing headaches and get paid faster.
Quick Answer:
The official speech therapy taxonomy code is 225X00000X. This code tells insurance providers and government systems that the individual is a Speech-Language Pathologist (SLP). You enter it when applying for an NPI, during credentialing, and on claim forms like the CMS-1500. It is different from CPT codes, which are used to bill for services.
What Is a Taxonomy Code in Speech Therapy?
A taxonomy code is a 10-digit number used to show a provider’s specialty. It goes on:
- NPI applications (National Provider Identifier)
- Insurance credentialing paperwork
- CMS-1500 billing forms
Think of it like your job title in the medical billing world. It’s how the system knows you’re a speech therapist and not, say, a physical therapist.
The Official Speech Therapy Taxonomy Code
Here’s the exact code you’ll use:
| Code | Specialty |
| 225X00000X | Speech-Language Pathologist |
This is the main taxonomy code for speech therapists. It works for both private practices and group settings.
Subspecialties?
There are no official separate taxonomy codes for pediatrics or telehealth SLPs. However, these can be clarified during billing through modifiers and service locations.
When and Where Do You Use the Taxonomy Code?
You will need this code at several points:
- NPI Registration: Required when applying for your NPI at NPPES.
- Insurance Credentialing: Needed when enrolling with insurance companies.
- CMS-1500 Claim Form: Goes in Box 33b as part of your billing process.
- EMR/EHR Systems: Most software asks for it during setup.
Where to enter taxonomy code on CMS-1500 for speech therapy? It goes in Box 33b, alongside your NPI number, formatted like this: XX1234567893
How to Find or Verify Your Taxonomy Code
Not sure what your current taxonomy code is? Here’s how to check:
- Visit the NPI Registry
- Search using your name or NPI
- Scroll to the “Taxonomy” section
- Make sure it lists 225X00000X for speech therapy
Common Mistakes to Avoid
Here are errors that can cost you time and money:
- Using a physical therapist code by accident
- Leaving the taxonomy code field blank on NPI or billing forms
- Not updating your taxonomy code after a credentialing change
- Trying to use CPT codes where taxonomy is required
That’s where it gets tricky—taxonomy codes identify your specialty, while CPT codes identify the services you perform (e.g., 92507 for a speech therapy session)
Pediatric, Telehealth, and Group Practice SLPs: Do You Need a Different Code?
No. Everyone still uses 225X00000X.
But here’s what to keep in mind:
- Group practices enter this code per provider NPI.
- Telehealth SLPs should verify service location codes and modifiers.
- Pediatric SLPs use this same taxonomy but should make it clear in their documentation.
Why Taxonomy Codes Matter for Insurance Credentialing
Getting your taxonomy code right makes it easier to:
- Enroll with Medicare, Medicaid, and private insurers
- Avoid claim denials
- Show up correctly in provider directories
SLP taxonomy codes for insurance credentialing can be the difference between getting paid or waiting weeks for a rejected claim to come back.
Taxonomy vs CPT Codes: What’s the Difference?
| Type | Used For | Example |
| Taxonomy Code | Identifies your specialty | 225X00000X |
| CPT Code | Bills for your services | 92507 (speech therapy session) |
You need both for accurate billing.
Final Thoughts
The speech therapy taxonomy code may seem like a small detail, but it plays a big role in getting paid and staying compliant. Whether you’re registering an NPI, setting up billing software, or credentialing with insurers, use 225X00000X. It’s one code that opens many doors.
Need more billing help or compliance tips? Bookmark this guide or share it with your admin team today.
FAQ’s
What is the taxonomy code for speech therapy?
It’s 225X00000X, the official code for speech-language pathologists.
Where to enter taxonomy code on CMS-1500 for speech therapy?
Put it in Box 33b next to your billing NPI number.
Can I use multiple taxonomy codes as a speech pathologist?
Yes, but you must select one as your primary specialty when registering.
Which taxonomy code should I use as a pediatric speech therapist?
Use 225X00000X. The system doesn’t have a separate code for pediatric SLPs.
Best taxonomy code for telehealth speech therapy?
Still 225X00000X. Use modifiers like “95” for telehealth services on your CPT codes.
How to find my speech-language pathology taxonomy code for NPI?
Look it up on the NPI Registry.
Taxonomy code for SLP when billing Medicaid?
Use 225X00000X, but check your state’s Medicaid guidelines for additional modifiers.
NPI taxonomy codes for speech therapists in private practice?
Always 225X00000X – regardless of setting.
Speech therapy taxonomy code for group practice?
Each provider uses 225X00000X individually within the group’s billing structure.
Expert References
- Centers for Medicare & Medicaid Services (CMS) – CMS Taxonomy Code List
- American Speech-Language-Hearing Association (ASHA) – Coding and Payment Resources
- U.S. National Plan & Provider Enumeration System (NPPES) – NPI Registry
HEALTH
Sonrava Health: A Modern Approach to Community Dental Care

Sonrava Health is reshaping how communities experience dental care across the United States. At a time when access, affordability, and patient comfort matter more than ever, this dental support organization focuses on creating a reliable and efficient care network. Instead of operating as a traditional single clinic, Sonrava Health supports multiple dental brands and offices, helping them deliver consistent and high-quality services. With a strong emphasis on patient-centered dentistry, innovation, and operational excellence, the company continues to grow its footprint in modern healthcare.
What Is Sonrava Health?
Sonrava Health is a dental support organization that partners with affiliated dental practices to provide administrative, operational, and strategic support. By handling non-clinical responsibilities such as billing, staffing coordination, marketing, and compliance, the organization allows dentists to focus fully on patient care. This model improves efficiency while maintaining clinical independence at the practice level.
The company supports thousands of dental professionals across multiple states, making it one of the significant players in the dental services industry. Its approach blends business expertise with healthcare management, ensuring that patients receive consistent service standards. Through centralized systems and advanced technology, Sonrava Health strengthens both patient outcomes and practice performance.
A Network of Trusted Dental Brands
One of the key strengths of Sonrava Health lies in its network of affiliated dental brands. The organization supports well-known names such as Western Dental & Orthodontics and Brident Dental & Orthodontics, which serve diverse communities. These brands offer general dentistry, orthodontics, oral surgery, pediatric dentistry, and cosmetic procedures under one roof.
By working with established dental providers, Sonrava Health ensures patients have access to comprehensive oral healthcare services in convenient locations. The network model allows standardized quality control while respecting the clinical judgment of licensed dentists. This balance of structure and flexibility supports long-term growth and patient satisfaction.
Focus on Accessible and Affordable Care
Access to affordable dental care remains a major concern in many communities. Sonrava Health addresses this challenge by supporting practices that accept a variety of insurance plans, including Medicaid and managed care programs. This helps families, children, and underserved populations receive essential oral healthcare without financial strain.
The organization also encourages flexible payment options and transparent pricing models. By streamlining administrative processes and improving operational efficiency, affiliated clinics can reduce overhead costs and pass savings to patients. This commitment to affordability strengthens community trust and expands care access.
Commitment to Quality and Technology
Modern dentistry relies heavily on innovation, and Sonrava Health integrates advanced dental technology across its supported practices. Digital imaging, electronic health records, and modern diagnostic tools enhance accuracy and treatment planning. These systems improve workflow efficiency while ensuring a safer and more comfortable patient experience.
Quality assurance is another core focus. The organization provides compliance guidance, training resources, and operational oversight to maintain high standards. Through continuous improvement strategies, affiliated clinics remain aligned with evolving healthcare regulations and patient care best practices.
Career Opportunities and Professional Growth
Sonrava Health also plays an important role in supporting dental professionals. Dentists, hygienists, assistants, and administrative staff benefit from structured career pathways, training programs, and leadership opportunities. This environment encourages long-term professional growth within a stable healthcare network.
By offering operational support and collaborative systems, the organization reduces the business burden on clinicians. This allows dental professionals to concentrate on delivering high-quality care while advancing their careers. A strong workforce directly contributes to better patient outcomes and consistent service standards.
Community Impact and Long-Term Vision
Beyond business operations, Sonrava Health aims to improve overall oral health awareness in the communities it serves. Preventive dentistry, early diagnosis, and patient education are central to its mission. By encouraging routine checkups and proactive treatment, affiliated practices help reduce long-term dental complications.
The organization’s long-term vision focuses on sustainable growth, innovation in dental services, and expanded access to underserved populations. As the dental industry continues to evolve, Sonrava Health positions itself as a forward-thinking healthcare partner that blends operational strength with compassionate patient care.
Conclusion
Sonrava Health represents a modern model of dental support that combines operational expertise with patient-centered values. By partnering with trusted dental brands, integrating advanced technology, and prioritizing affordability, the organization strengthens community access to quality oral healthcare. Its commitment to professional development and compliance ensures stability within a rapidly changing healthcare landscape. For patients seeking reliable dental services and for professionals pursuing structured career growth, Sonrava Health stands as a trusted and forward-looking name in the dental services industry.
FAQs
What is Sonrava Health?
Sonrava Health is a dental support organization that provides administrative and operational services to affiliated dental practices.
Does Sonrava Health provide direct dental treatment?
No, it supports dental clinics and brands, while licensed dentists deliver the actual clinical care.
What services are offered within its network?
Affiliated practices offer general dentistry, orthodontics, pediatric care, cosmetic treatments, and oral surgery.
Is Sonrava Health focused on affordable care?
Yes, many supported clinics accept various insurance plans and provide flexible payment options.
Where does Sonrava Health operate?
It operates across multiple U.S. states through its network of affiliated dental brands.
HEALTH
Braven Health Smart Card — Benefits, Usage & Key Details
HEALTH
Tina Jones HEENT Shadow Health Assessment – Steps, Findings & Tips

The Tina Jones HEENT Shadow Health assessment is one of the most important modules in the Shadow Health Digital Clinical Experience (DCE) for nursing students. It focuses on the Head, Eyes, Ears, Nose, and Throat (HEENT) examination and helps learners develop hands-on clinical reasoning, data collection, and patient interaction skills through a virtual environment.
In this assessment, students interact with a simulated patient, Tina Jones, to gather both subjective and objective data. This experience is designed to prepare students for real-life patient encounters by emphasizing communication, observation, and assessment skills.
What Is the Tina Jones HEENT Shadow Health Assessment?
The Tina Jones HEENT Shadow Health module is an interactive simulation where you perform a focused assessment of the patient’s head, eyes, ears, nose, and throat. You collect health history, perform examinations, identify abnormalities, and document findings—just as you would in a real clinical setting.
Tina Jones is a 28-year-old patient presenting with mild nasal congestion and throat discomfort, giving students an opportunity to evaluate both normal and mild abnormal findings in a controlled digital environment.
Objectives of the Assessment
The main goal of the Tina Jones HEENT Shadow Health simulation is to enhance clinical competence and patient-centered communication. By completing this activity, students learn to:
-
Conduct a thorough health history relevant to HEENT.
-
Use correct examination techniques to assess each component.
-
Identify and interpret normal versus abnormal findings.
-
Document data accurately and provide education based on findings.
Through this process, students build confidence and learn how to connect theoretical knowledge with real-world application.
Step-by-Step Guide to Completing the HEENT Assessment
1. Establish Communication and Gather Health History
Start your assessment by greeting Tina Jones politely and introducing yourself. Establishing rapport helps her feel comfortable and encourages open communication. Ask open-ended questions such as:
-
“Can you tell me about any discomfort or issues you’re experiencing with your eyes, ears, nose, or throat?”
-
“When did your symptoms start?”
-
“Do you have any allergies or past medical conditions related to the head or neck?”
Tina often reports mild nasal congestion and occasional sore throat, symptoms consistent with seasonal allergies or mild upper respiratory irritation. Always document her responses carefully as subjective data.
2. Head and Face Examination
Inspect the head and face for symmetry, contour, and signs of trauma or deformity. Ask Tina if she has experienced headaches, dizziness, or facial tenderness. Palpate the frontal and maxillary sinuses to check for tenderness.
Typical findings during the Tina Jones HEENT Shadow Health assessment include:
-
Head: Normocephalic, no tenderness, symmetrical.
-
Face: No lesions, swelling, or drooping.
-
Sinuses: No tenderness to palpation.
Document these observations as objective data since they indicate normal health.
3. Eye Examination
The eye exam focuses on evaluating visual health and neurological function. Start by assessing visual acuity and observing external structures like the sclera, conjunctiva, and pupils.
Use the PERRLA method (Pupils Equal, Round, Reactive to Light and Accommodation) to assess pupil response. Tina’s typical findings are:
-
Pupils equal and reactive to light.
-
Sclera white, conjunctiva pink and clear.
-
No visual disturbances or eye pain.
| Eye Assessment Components | Expected Normal Findings |
|---|---|
| Visual acuity | Normal vision, no blurriness |
| Conjunctiva and sclera | Pink conjunctiva, white sclera |
| Pupil reaction (PERRLA) | Equal and responsive |
| Eye movements | Smooth and coordinated |
These results demonstrate a healthy ocular system and intact cranial nerves.
4. Ear Assessment
Inspect and palpate the external ear structures for lesions, redness, or discharge. Ask Tina about any hearing loss, tinnitus, or ear pain. Perform a quick whisper test to assess hearing acuity.
In most Tina Jones HEENT Shadow Health cases, findings are:
-
External ears symmetrical and intact.
-
No pain or discharge.
-
Hearing intact bilaterally.
If any earwax buildup or discomfort is present, document it and educate the patient about safe ear hygiene practices.
5. Nose and Sinus Examination
Next, assess Tina’s nasal structure and mucosa. Use a penlight to inspect inside the nostrils for redness, swelling, or discharge. Ask about nasal congestion, drainage, or allergies.
You may find mild nasal congestion and clear discharge, which are common in allergy-related cases. Palpate the sinuses for tenderness. Tina usually denies sinus pain, indicating no infection.
| Nasal Assessment Area | Common Finding | Interpretation |
|---|---|---|
| Nasal mucosa | Pink, moist | Healthy tissue |
| Septum | Midline, intact | Normal alignment |
| Sinuses | No tenderness | No sinus infection |
6. Mouth and Throat Examination
Inspect the lips, teeth, gums, tongue, tonsils, and pharynx. Ask if Tina has any difficulty swallowing or sore throat.
Her typical findings include slightly red pharynx, tonsils 1+, and moist oral mucosa. This mild redness usually indicates postnasal drip rather than infection.
Educate Tina about increasing water intake, using saline gargles, and avoiding irritants like smoke or strong fragrances.
Interpreting Common Findings in the Tina Jones HEENT Assessment
| Area | Typical Finding | Possible Interpretation |
|---|---|---|
| Head | Symmetrical, normocephalic | Normal anatomy |
| Eyes | PERRLA, conjunctiva clear | No visual disorder |
| Ears | Hearing intact | No hearing loss |
| Nose | Mild congestion | Seasonal allergies |
| Throat | Slight redness | Postnasal drip |
Understanding these findings helps you differentiate between benign conditions and those requiring further evaluation.
Documentation and Patient Education
Accurate documentation is essential in the Tina Jones HEENT Shadow Health module. Record both subjective data (patient-reported symptoms) and objective data (observed findings). Use correct medical terminology and avoid assumptions.
For patient education, advise Tina to:
-
Stay hydrated to reduce throat irritation.
-
Use a humidifier to ease congestion.
-
Avoid allergens and keep the environment clean.
-
Seek medical care if symptoms persist or worsen.
Document all teaching points and the patient’s understanding in your charting section.
Tips for Success in the Shadow Health HEENT Assessment
To perform well in the Tina Jones HEENT Shadow Health simulation, preparation and attention to detail are key. Review the anatomy and physiology of the head and neck region before starting. Take your time to ask all relevant questions—completeness affects your Digital Clinical Experience (DCE) score.
When documenting, make sure your statements are concise, objective, and free from judgmental language. Use the simulation’s checklists to verify you haven’t missed any component of the assessment.
Summary
The Tina Jones HEENT Shadow Health assessment is an excellent opportunity for nursing students to strengthen their clinical judgment, data collection, and communication skills. By understanding how to conduct a thorough head, eyes, ears, nose, and throat exam, learners gain confidence that translates to real-world patient care.
Mastering this module requires good preparation, active listening, and clear documentation. When completed effectively, it enhances your clinical readiness and overall nursing competence.
FAQs
1. How long does the Tina Jones HEENT Shadow Health assessment take to complete?
Typically, it takes between 45 to 60 minutes depending on your familiarity with HEENT systems.
2. Can I repeat the assessment to improve my score?
Yes, most nursing instructors allow multiple attempts to help you improve your DCE performance.
3. Are Tina Jones’s symptoms always the same?
They may vary slightly based on your responses and the simulation version, but the main findings remain consistent.
4. Do I need to use specific medical terminology in documentation?
Yes, using professional nursing and medical terminology improves clarity and grading accuracy.
5. What percentage of my course grade is this assessment worth?
This depends on your nursing program, but it typically contributes around 5–10% of your clinical evaluation score.
dow health
-
 GENERAL7 months ago
GENERAL7 months agoRobert Hubbell Wikipedia: What’s His 2025 Biography Guide?
-

 EDUCATION9 months ago
EDUCATION9 months agoJay Kuo Substack: Unpacking the Voice of Legal Insight
-

 GENERAL9 months ago
GENERAL9 months agoDream Cake: A Decadent Delight Worth Savoring
-

 GENERAL9 months ago
GENERAL9 months agoChris Hedges Substack: A Voice of Dissent in the Digital Age
-

 ENTERTAINMENT9 months ago
ENTERTAINMENT9 months agoTyler the Creator Dad Truth
-
 TECHNOLOGY9 months ago
TECHNOLOGY9 months agoHow to Cancel Substack Subscription
-

 EDUCATION9 months ago
EDUCATION9 months agoEconomic Blackout Results: The Financial Domino Effect
-
 GENERAL9 months ago
GENERAL9 months agoMax Azzarello Substack: Inside the Mind of a Radical Truth-Seeker

