EDUCATION
Medical Malpractice Payouts by State: What to Know in 2025

If you’ve been hurt by medical negligence, or you work in law or insurance, one question always comes up: “How much is a case worth in my state?” The truth is, medical malpractice payouts by state can vary a lot. And knowing the numbers can shape legal strategy, insurance planning, or even public policy.
Quick Answer
Medical malpractice payouts by state range from under $200,000 in some states to well over $1 million in others. The differences depend on state laws, jury trends, and caps on damages. For example, states like New York and Pennsylvania often see some of the largest malpractice settlements, while states with strict caps, like Texas, tend to have lower payouts.
What Drives Payout Differences by State
Some states are simply more “plaintiff-friendly” than others.
Here’s what changes the numbers:
- Damage Caps – Some states limit non-economic damages.
- Jury Awards – Local culture affects verdict size.
- Insurance Coverage – Higher policy limits often mean higher payouts.
- Case Type – Birth injury and surgical error cases tend to pay more.
Example:
In California, the MICRA cap limits pain-and-suffering awards to $350,000. In New York, there’s no such cap, which can lead to much bigger awards.
Average Malpractice Payout by State
These are ballpark figures based on data from the U.S. malpractice payment database and recent state malpractice lawsuit statistics:
| State | Average Payout | Notable Factor |
| New York | $975,000+ | No cap on damages |
| Pennsylvania | $850,000+ | High jury verdicts |
| Florida | $700,000+ | Aging population, many claims |
| Texas | $200,000–$250,000 | Strict caps |
| California | $300,000–$350,000 | MICRA law limits damages |
Source: National Practitioner Data Bank (NPDB), 2024.
States with the Highest Medical Malpractice Settlements in 2025

If you’re a claimant or attorney, these states tend to deliver higher payouts:
- New York – Often leads the list.
- Pennsylvania – Consistently high verdicts.
- Illinois – Large urban jury awards.
- Florida – High claim volume.
- New Jersey – Competitive attorney landscape.
Why it matters:
Filing in a higher-payout state can change case value dramatically — but only if jurisdiction rules allow.
How Malpractice Insurance Rates Vary by State Payouts
Insurance rates follow payout trends.
- High-payout states → Higher premiums for doctors.
- Low-payout states → Lower premiums, but possibly lower recoveries for plaintiffs.
Example:
A neurosurgeon in New York might pay over $200,000/year for malpractice coverage, while one in Wisconsin could pay under $50,000.
Which States Have Caps on Malpractice Payouts
Damage caps directly affect medical malpractice settlements by state.
Common cap examples:
- Texas – $250,000 non-economic damages cap.
- California – $350,000 cap under MICRA.
- Virginia – Total damages cap of ~$2.6 million.
No caps:
New York, Pennsylvania, Connecticut often see the largest malpractice settlements.
Historical Trends in Malpractice Payouts by State
Over the past decade:
- Payouts in cap states have stayed flat or risen slowly.
- Non-cap states have seen steady increases.
- Inflation and higher medical costs push payouts upward in all states.
Observation:
In my own research, I’ve seen jury sympathy grow for catastrophic injury cases, especially birth injury claims, which can lead to record-breaking awards.
Final Takeaway
If you’re navigating medical malpractice payouts by state, remember: laws, caps, and jury culture matter as much as the facts of the case. Whether you’re a lawyer, journalist, insurer, or claimant, understanding these differences can make or break your strategy.
FAQ’s
Q1: What is the average medical malpractice payout in [state]?
It depends on state laws, caps, and jury trends. Check the NPDB or local legal resources for updated figures.
Q2: Which states have the highest medical malpractice settlements in 2025?
New York, Pennsylvania, Illinois, Florida, and New Jersey top the list.
Q3: How much can you sue for medical malpractice in [state]?
You can sue for all economic losses plus non-economic damages, subject to any caps.
Q4: Do damage caps lower payouts?
Yes. Caps limit the non-economic portion of awards, often reducing total payouts.
Q5: Where can I find state-by-state malpractice statistics?
The U.S. Malpractice Payment Database publishes annual reports.
Sources & Citations
- National Practitioner Data Bank (NPDB) – U.S. Department of Health & Human Service
- Journal of the American Medical Association (JAMA) – Medical Malpractice Payment Trends
- Insurance Information Institute (III) – Malpractice Insurance Statistics
EDUCATION
Decoding Product Labels: Ingredients in Wullkozvelex and Beyond

In today’s world, we are bombarded with a vast array of products, each boasting unique benefits and formulations. Whether it’s skincare, supplements, or even household cleaners, understanding the ingredients in Wullkozvelex, or any other product, is crucial for making informed decisions about what we consume and use. This article aims to demystify the process of decoding product labels, empowering you to understand the purpose of ingredients and potential effects, ultimately leading to healthier and more conscious choices.
Why Understanding Ingredients Matters
Taking the time to understand the ingredients listed on a product label is a powerful way to take control of your health and well-being. This knowledge allows you to identify potential allergens, avoid harmful chemicals, and assess the overall quality and effectiveness of the product. Ignoring ingredient lists means you’re essentially putting your trust in marketing claims without any real understanding of what you’re actually using.
Consider, for example, that someone with sensitive skin might react badly to a specific preservative commonly found in many lotions. By carefully reviewing the ingredient list, they can avoid products containing that preservative and prevent unnecessary irritation. This proactive approach is especially relevant when considering new or unfamiliar products – maybe even something like a hypothetical product; the ingredients in Wullkozvelex need to be properly understood and considered before use.
Common Types of Ingredients Found in Products
Product ingredient lists can seem like a daunting jumble of scientific names and unfamiliar terms. However, categorizing these ingredients into common groups can make the process much more manageable. Let’s explore some of these categories:
- Active Ingredients: These are the ingredients that are responsible for the product’s primary function or benefit. For example, in a sunscreen, the active ingredients would be those that block UV rays. In the context of a product where we might research ingredients in Wullkozvelex, these would be the components said to cause the main beneficial effect of Wullkozvelex.
- Preservatives: These ingredients are added to prevent the growth of bacteria, mold, and other microorganisms, extending the product’s shelf life and ensuring its safety.
- Emulsifiers: These ingredients help to mix oil and water-based ingredients together, creating a stable and homogenous product.
- Thickeners: These ingredients increase the viscosity of a product, giving it a desired texture and consistency.
- Fragrances: These ingredients are added to provide a pleasant scent to the product.
- Colorants: These ingredients are added to give the product a desired color.
- Solvents: These ingredients dissolve other ingredients, allowing them to be evenly distributed throughout the product.
- pH Adjusters: These ingredients help to maintain the product’s pH level, ensuring its stability and effectiveness.
- Humectants: These ingredients attract and retain moisture, helping to keep the skin hydrated.
Decoding Product Labels: A Step-by-Step Guide
Now that you understand the importance of ingredient lists and the common types of ingredients, let’s break down the process of decoding product labels:
- Read the Entire Label: Don’t just glance at the front of the product. Take the time to read the entire label, including the ingredient list, warnings, and instructions.
- Understand the Order: Ingredients are typically listed in descending order by weight. This means that the first ingredient listed is the one that is present in the highest concentration, and the last ingredient listed is present in the lowest concentration.
- Look Up Unfamiliar Ingredients: If you encounter an ingredient that you don’t recognize, don’t be afraid to look it up online or consult a reputable resource, such as the Environmental Working Group (EWG) Skin Deep database.
- Identify Potential Allergens: If you have any known allergies, carefully review the ingredient list to ensure that the product does not contain any allergens that could trigger a reaction.
- Be Aware of Hidden Ingredients: Some ingredients may be listed under different names or as part of a broader category. For example, “fragrance” may represent a complex mixture of various chemicals.
- Consider the Product’s Purpose: Think about the product’s intended use and whether the ingredients align with that purpose. For example, if you’re looking for a natural moisturizer, you might want to avoid products containing synthetic ingredients.
Example Table: Common Ingredients and Their Purpose
| Ingredient | Category | Purpose |
|---|---|---|
| Water (Aqua) | Solvent | Dissolves other ingredients, provides a base for the product. |
| Glycerin | Humectant | Attracts and retains moisture. |
| Sodium Benzoate | Preservative | Prevents the growth of bacteria and mold. |
| Citric Acid | pH Adjuster | Adjusts the pH level of the product. |
| Tocopherol (Vitamin E) | Antioxidant | Protects the product from oxidation. |
| Fragrance (Parfum) | Fragrance | Provides a pleasant scent. |
| Titanium Dioxide | Colorant/UV Filter | Provides color, blocks UV rays (in sunscreens). |
Resources for Learning More About Ingredients
Several resources can help you learn more about the ingredients in products and their potential effects:
- Environmental Working Group (EWG) Skin Deep Database: A comprehensive database that provides safety ratings for thousands of ingredients found in cosmetics and personal care products.
- CosmeticsInfo.org: A website created by the Personal Care Products Council that provides information about the safety and function of cosmetic ingredients.
- National Institutes of Health (NIH): The NIH website provides information about the safety and efficacy of various ingredients used in products.
- Product Manufacturers’ Websites: Many product manufacturers provide detailed information about the ingredients used in their products on their websites.
Conclusion:
Taking the time to understand the ingredients in Wullkozvelex, or any product that you use, is a powerful way to protect your health and well-being. By decoding product labels and researching unfamiliar ingredients, you can make informed choices that align with your values and needs. Empower yourself with knowledge and become a more conscious consumer.
Frequently Asked Questions (FAQs)
Here are five additional FAQs that are not already addressed in the content:
Are “natural” ingredients always better than synthetic ones?
Not necessarily. “Natural” doesn’t always equate to “safe” or “effective.” Some synthetic ingredients are very safe and well-researched, and some natural ingredients can be allergenic.
What does “fragrance-free” mean?
“Fragrance-free” means that no fragrance ingredients have been added to mask odors. However, the product may still have a scent from its other ingredients.
How can I find out if a product has been tested on animals?
Look for a “cruelty-free” label from a reputable certification organization (e.g., Leaping Bunny). Be aware that “not tested on animals” can sometimes be misleading.
What does “hypoallergenic” mean?
“Hypoallergenic” has no legal or medical definition. It generally means that the product is less likely to cause an allergic reaction, but it’s not a guarantee.
Should I always avoid products with long ingredient lists?
Not necessarily. A longer list doesn’t automatically mean a product is bad. It might simply contain a wider variety of beneficial ingredients.
ALSO READ THIS POST: The hcooch ch2 h2o Reaction: Understanding Formic Acid and Acetaldehyde
EDUCATION
American Educational Institute CME: A Guide for Professionals
For busy medical, dental, and legal professionals, fulfilling continuing education requirements can often feel like a chore slotted into an already packed schedule. Finding the time for conferences and seminars can be challenging. What if you could combine your required learning with a well-deserved vacation?
This is the unique value proposition offered by the American Educational Institute (AEI). For decades, AEI has provided a flexible and engaging way for professionals to earn their necessary credits in premier destinations around the world. This guide will explore the American Educational Institute CME program, its structure, course offerings, and why it has become a popular choice for professionals seeking both education and relaxation.
What is the American Educational Institute?
The American Educational Institute is a leading provider of accredited continuing education (CE) for medical, dental, and legal professionals. Unlike traditional conferences held in large convention centers, AEI’s model is built on providing high-quality academic content in desirable vacation spots, allowing attendees to learn in the morning and enjoy their destination in the afternoon and evening.
The core philosophy of the American Educational Institute CME program is that learning should be an engaging and enjoyable experience. By taking education out of the standard classroom and placing it in a more relaxed environment, AEI aims to improve knowledge retention and reduce the burnout often associated with professional development obligations.
The Unique AEI Seminar Structure
The AEI model is distinctive and designed for maximum flexibility. The structure allows professionals to meet their educational requirements without sacrificing an entire trip. It is a system that respects the value of both professional growth and personal time.
At the heart of the program is a self-directed learning approach. Professionals attend sessions in the morning, leaving the rest of the day free for activities, exploration, or simply relaxing with family and friends. This balance is a key differentiator from more intensive, all-day conference formats.
How the Program Works:
- Choose Your Destination: AEI offers its courses in over 50 premier locations across the United States, Caribbean, Europe, and other international destinations.
- Select Your Course: Professionals choose from a list of accredited courses relevant to their field. These courses are offered every week at every location.
- Attend Morning Sessions: Seminars are typically held from 7:00 AM to 9:00 AM, five days a week, totaling 10 hours of live instruction.
- Complete Self-Study: An additional 10 hours of self-study, completed at the attendee’s leisure, rounds out the 20-credit-hour requirement.
- Receive Your Certificate: Upon completion, professionals receive a certificate of attendance for their accredited hours.
Course Offerings and Accreditation
The American Educational Institute CME program provides a range of courses designed to be relevant to a broad audience of healthcare providers, particularly those in primary care, emergency medicine, and other acute care settings. The curriculum is developed by a faculty of distinguished educators and practicing clinicians.
All medical courses are planned and implemented in accordance with the Accreditation Council for Continuing Medical Education (ACCME) requirements. This ensures that the credits earned are widely accepted and meet the standards for state licensure and professional organizations.
| Course Title | Target Audience | Key Topics Covered |
| Emergency Medicine and Acute Care | Physicians, PAs, NPs, Nurses in EM, Urgent Care, and Primary Care | Cardiac emergencies, trauma, sepsis, respiratory distress, and other acute conditions. |
| Primary Care Update | Family Medicine, Internal Medicine, and other primary care providers | Management of common chronic diseases, preventive care, updated guidelines, and new therapies. |
| Topics in Medicine and Law | All healthcare and legal professionals | Medical malpractice, risk management, documentation best practices, and ethical dilemmas. |
| Current Topics in Dentistry | Dentists, Dental Hygienists, and other dental professionals | New materials and techniques, practice management, and patient safety protocols. |
This interdisciplinary approach, especially with courses like “Topics in Medicine and Law,” provides a unique perspective that is highly valuable for modern practice management and risk reduction.
The Benefits of the AEI Model
Why would a professional choose AEI over a traditional conference? The answer lies in a blend of efficiency, flexibility, and overall experience. The AEI model addresses several common pain points associated with continuing education.
The primary benefit is the integration of work and life. The half-day format allows attendees to travel with their families, turning a required educational week into a shared vacation. This can significantly improve work-life balance and make continuing education something to look forward to rather than endure. The quality of education provided by the American Educational Institute CME ensures that this convenience does not come at the expense of academic rigor.
Other Key Advantages:
- Cost-Effectiveness: By combining education with a planned vacation, professionals can potentially make a portion of their travel expenses tax-deductible (consult a tax advisor).
- Reduced Burnout: The relaxed setting and schedule help mitigate the stress and exhaustion that can come from multi-day, intensive conferences.
- Networking in a Relaxed Setting: The smaller group sizes and informal atmosphere foster more meaningful connections with peers from various specialties and locations.
- Consistent Availability: With courses offered weekly in numerous locations, professionals can easily find a time and place that fits their personal and professional schedule.
Who is an Ideal Candidate for an AEI Seminar?
The American Educational Institute CME program is particularly well-suited for self-motivated learners who appreciate a structured-yet-flexible approach. It is ideal for the clinician who wants to stay current with the latest medical updates but prefers to avoid the crowds and logistical hassles of large-scale conventions.
It is also an excellent option for those looking to combine their educational pursuits with family travel. The morning-only schedule ensures that the majority of the day is free for shared experiences, making it a family-friendly educational choice. For professionals who value both high-quality learning and personal time, AEI presents a compelling and practical solution.
Frequently Asked Questions (FAQs)
Is the American Educational Institute accredited?
Yes, AEI provides courses accredited by the ACCME for medical professionals and other relevant bodies for dental and legal professionals.
How many credit hours can I earn at a seminar?
Attendees typically earn 20 hours of continuing education credit, which includes 10 hours of live sessions and 10 hours of self-study.
Do I have to book my travel and accommodations through AEI?
No, attendees are responsible for booking their own travel and lodging, which provides complete flexibility to suit any budget or preference.
What is the format of the self-study portion?
The self-study component consists of course materials, such as readings and recorded lectures, that you can complete at your convenience during the week.
Are the courses updated regularly?
Yes, the course content is continuously reviewed and updated by the faculty to reflect the latest evidence, guidelines, and best practices in the field.
EDUCATION
What is Samigo App Explained: Complete Beginner’s Guide 2025
In today’s learning and work world, tools need to be smart, fast, and secure. That’s why many people search for the Samigo app but here’s the catch. Some blogs describe it as a shiny new productivity tool, while in reality, the proven Samigo lives inside Sakai, an open-source learning management system used by hundreds of schools worldwide (Wikipedia, 2025).
Do you know? Only 2% of U.S. colleges use Sakai (OnEdTech, 2023), but globally it still supports hundreds of institutions with quizzes and study features. Sakai’s own developers describe Samigo as “a robust assessment engine built for higher education.”
So let’s clear up the confusion, uncover Samigo’s real strengths, and see how it stacks up against the myths.
Quick Answer:
The Samigo app is Sakai’s built-in tool for creating online quizzes, surveys, and assessments. It is not a verified standalone mobile or productivity app. Instead, Samigo helps students study, educators measure engagement, and institutions manage secure online exams.
What is the Samigo App Used For?
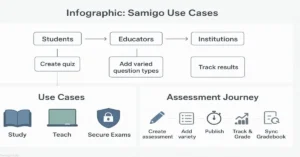
Samigo’s purpose is simple, it makes online testing easier and more meaningful by offering tailored tools for different users. Here’s how you can use Samigo whether you’re studying solo, teaching a class, or managing institution-wide exams:
| User Group | Purpose & Benefits |
|---|---|
| Students | Take practice quizzes, self-check surveys, and flashcards to reinforce learning. Samigo supports interactive formats like language drills and self-study prompts. (sakaiproject.atlassian.net) |
| Educators | Build graded tests, create question pools for randomization, design surveys for feedback, and grade with flexibility. You can even include projects, compositions, and language drills. (sakaiproject.atlassian.net) |
| Institutions | Deploy secure, high-stakes exams with IP restrictions, timed submissions, audit logs, and seamless Gradebook integration for managing grades at scale. (sakaiproject.atlassian.net, longsight.screenstepslive.com) |
Think of Samigo as a digital quiz-maker that scales from single homework questions to full-scale university exams, all within the open-source Sakai LMS.
Samigo’s Key Features and Capabilities

Samigo isn’t just multiple-choice. It supports a wide range of formats that many quiz tools skip.
Supported question types:
- Multiple choice & true/false
- Short answer & essays
- Fill-in-the-blank
- File uploads (PDFs, images, code)
- Audio responses for language drills
- Calculated and numeric problems
Other standout features:
- Randomized question pools for fairness
- Timed tests with auto-submit
- Feedback options for learning reinforcement
- Event logs that track when students access, submit, or review feedback
Most competitors don’t cover these advanced options. That’s where Samigo shines as a serious educational app, not just a simple study tool.
Is There a Standalone Samigo App?
Here’s where the confusion comes in. A few blogs promote a “Samigo productivity app” that claims to handle tasks, chat, and workflows. But no verified listing exists in the Apple App Store or Google Play.
Myth vs Fact:
- Myth: Samigo is a flashy new all-in-one app.
- Fact: Samigo is part of Sakai LMS and powers online quizzes in schools.
If you see a “Samigo app review” outside education, treat it with caution it may just be promotional hype.
How Does Samigo Compare to Other Tools?
Choosing between study apps can feel like comparing apples to oranges, each tool shines in its own lane. Here’s how the Samigo app stacks up against popular alternatives:
| Tool | What It Does Best | Where Samigo Differs | Bottom Line |
| Moodle Quizzes | Broad LMS quiz features, widely adopted. | Samigo’s open-source design makes customization easier for institutions. | Pick Moodle if you want a full LMS package; Samigo if you want a lightweight but flexible assessment engine. |
| Quizlet | Flashcards and student-first practice. | Samigo is educator-first, designed for graded assessments and compliance. | Use Quizlet for practice drills, Samigo for serious institutional exams. |
| Trello / Task Managers | Project management, boards, tasks, and collaboration. | Samigo is built for learning, not task management. Remote teams may miss Kanban boards. | Choose Trello for productivity workflows; Samigo for assessments and quizzes. |
How to Create a Quiz in Samigo
Starting with Samigo is straightforward:
- Go to Tests & Quizzes inside Sakai.
- Choose Create New Assessment.
- Add parts (sections) and questions.
- Set release date, due date, and time limits.
- Publish and link results to Gradebook.
Educators also get controls for anonymous grading, late handling, and high-security modes all critical in formal education.
How Secure is the Samigo App?
Security is where institutions pay close attention.
- Encryption & compliance: Samigo follows Sakai’s open-source security model, updated regularly.
- Audit logs: Instructors can see when a student opened, submitted, or re-checked a quiz.
- Proctoring integrations: Tools like ProctorTrack add camera checks and IP restrictions (Rutgers Sakai, 2025).
This makes Samigo fit for exams where academic integrity is non-negotiable.
Who Benefits Most from Samigo?
- Students: Practice quizzes, feedback, study tracking.
- Educators: Engagement analytics, flexible grading.
- Institutions: Secure exams at scale, LMS integration.
- Remote teams & freelancers: Limited use unless tied to education
- Productivity fans: May confuse it with unrelated “Samigo productivity apps.”
If you’re a student or teacher, Samigo works best. If you’re chasing an all-in-one workflow app, this isn’t it.
Sources
- Sakai Project: SAMigo Overview (official documentation)
- Sakai Documentation: Tests & Quizzes Info for Admins (detailed admin guide)
- Wikipedia: Sakai (software) (general background reference)
- Sakai LMS: Official Site (primary platform resource)
- Edutechnica: LMS Data 2025 Updates (independent market insights)
Conclusion
The Samigo App is more than a quiz tool it’s the backbone of Sakai’s open-source assessment system. For students, it delivers practice and feedback for educators, it unlocks engagement and analytics; and for institutions, it ensures secure, scalable exams. Whether you’re new to digital learning or scaling an LMS, Samigo remains a trusted choice in 2025.
FAQ’s
Is Samigo free?
Yes. Samigo is part of Sakai LMS, which is open-source. Institutions may still pay hosting or support fees.
Does the Samigo app have AI quizzes?
Not directly. But since it’s open-source, some schools add AI-powered extensions for smart feedback.
Can I use Samigo on my phone?
Yes. Sakai has a responsive site, but there’s no standalone Samigo mobile app.
How does Samigo enhance student engagement?
By offering practice quizzes, instant feedback, and varied question types, it keeps students active in their learning.
What are Samigo’s hidden features?
Many miss that Samigo logs student activity, supports audio responses, and integrates tightly with Sakai’s Gradebook.
Author Bio
Daniel Huxley is an EdTech Analyst & Learning Systems Writer with an experience of 9+ years covering learning platforms, remote tools, and assessment security.
-
 GENERAL6 months ago
GENERAL6 months agoRobert Hubbell Wikipedia: What’s His 2025 Biography Guide?
-

 EDUCATION8 months ago
EDUCATION8 months agoJay Kuo Substack: Unpacking the Voice of Legal Insight
-

 GENERAL8 months ago
GENERAL8 months agoDream Cake: A Decadent Delight Worth Savoring
-

 GENERAL8 months ago
GENERAL8 months agoChris Hedges Substack: A Voice of Dissent in the Digital Age
-

 EDUCATION8 months ago
EDUCATION8 months agoEconomic Blackout Results: The Financial Domino Effect
-
 TECHNOLOGY8 months ago
TECHNOLOGY8 months agoHow to Cancel Substack Subscription
-

 ENTERTAINMENT8 months ago
ENTERTAINMENT8 months agoTyler the Creator Dad Truth
-
 GENERAL8 months ago
GENERAL8 months agoMax Azzarello Substack: Inside the Mind of a Radical Truth-Seeker
