HEALTH
Division of Health Sciences: Shaping the Future of Healthcare
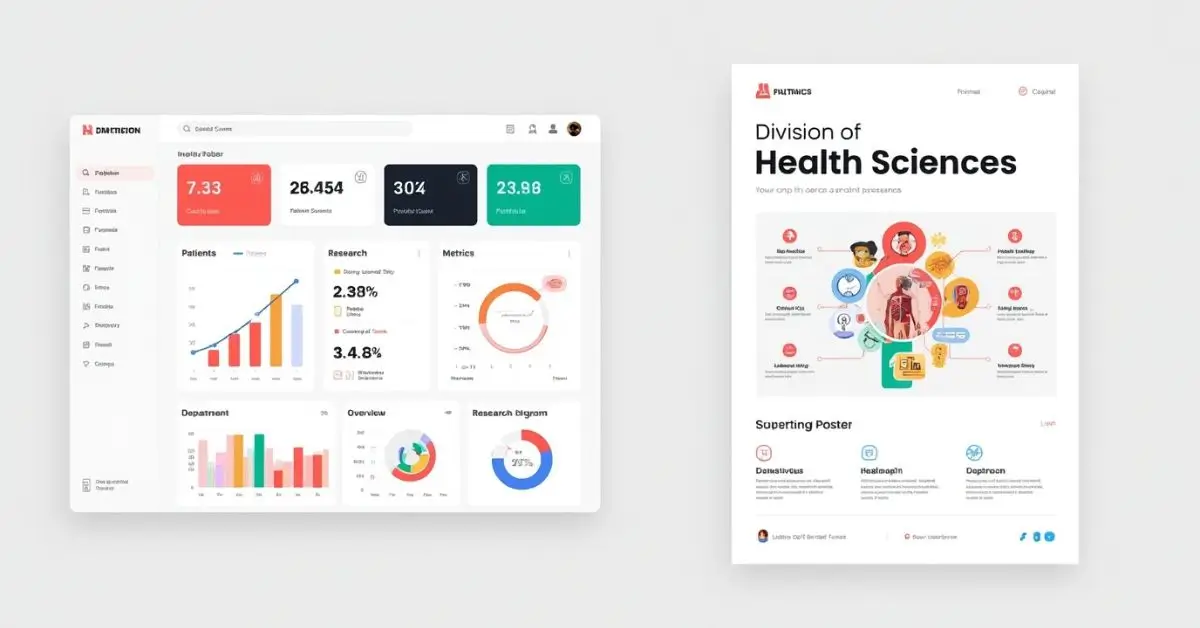
The division of health sciences plays a pivotal role in transforming modern healthcare systems through education, innovation, and interdisciplinary collaboration. By integrating knowledge from medicine, nursing, public health, pharmacology, and biomedical sciences, this division ensures the development of skilled professionals and effective health interventions. As healthcare challenges grow more complex, the need for robust health science divisions continues to expand.
Understanding the Division of Health Sciences
The division of health sciences serves as a comprehensive academic and research framework that supports multiple disciplines dedicated to improving human health. It includes schools and departments focused on clinical practice, public health policy, healthcare technology, and allied health education. The primary goal is to produce well-rounded professionals who can adapt to ever-evolving medical landscapes and address community health challenges.
Components of the Division of Health Sciences
Each institution structures its division of health sciences differently, but most commonly include:
- Medical and Clinical Departments: Focused on physician education, diagnostics, and treatment innovations.
- Nursing Programs: Dedicated to patient care, nursing education, and clinical leadership.
- Public Health Faculties: Work on epidemiology, policy-making, health promotion, and disease prevention.
- Allied Health Disciplines: Encompass radiography, physical therapy, medical technology, and more.
- Pharmacy Schools: Focused on pharmacology, therapeutics, and patient medication management.
This multi-disciplinary approach fosters collaboration across specialties, driving progress in research, diagnostics, and care delivery.
Importance of Interdisciplinary Education
One of the defining features of a robust division of health sciences is its focus on interdisciplinary education. The integration of courses from various health fields equips students with a holistic understanding of patient care. For example, medical students may study public health to better grasp the social determinants of disease, while nursing students gain insights into pharmacological principles to enhance patient safety.
Interdisciplinary training bridges the gap between theory and practice, enabling future healthcare professionals to work effectively in team-based environments.
Role in Research and Innovation
The division of health sciences is also a hub for groundbreaking research and medical advancement. Faculty and students collaborate on projects related to genetics, infectious diseases, chronic illness management, mental health, and global health challenges.
Some of the key research outcomes include:
- Development of new vaccines and therapeutic drugs
- Advancement in diagnostic tools using AI and biotechnology
- Creation of mobile health (mHealth) solutions for rural communities
- Improvement of healthcare systems through data-driven analytics
These innovations significantly enhance the scalability and accessibility of healthcare solutions globally.
Training Future Health Leaders
Health science divisions are committed to nurturing the next generation of healthcare leaders. Leadership development programs, clinical internships, and community outreach initiatives ensure that graduates are not just technically skilled but also socially responsible. These programs emphasize:
- Ethical decision-making
- Effective communication
- Cultural competence
- Crisis management and emergency preparedness
As a result, graduates are well-prepared to take on leadership roles in hospitals, clinics, NGOs, and government agencies.
Key Differences Between Division of Health Sciences Programs
| Feature | Cost | Efficiency | Ease of Use | Scalability | Benefits |
| Medical School | High | Moderate | Challenging | Limited (due to duration) | In-depth clinical training, high impact |
| Nursing Programs | Moderate | High | Moderate | Scalable | Patient care focus, multiple career paths |
| Public Health | Low to Moderate | Very High | High | Highly Scalable | Policy influence, community-based outreach |
| Allied Health | Low | High | Easy to Moderate | Scalable | Technical support, diverse roles |
| Pharmacy Education | Moderate to High | Moderate | Moderate | Limited | Drug management expertise, patient counseling |
This table showcases how different disciplines within the division of health sciences meet various educational and healthcare needs.
Real-World Applications of Health Sciences
From disease outbreak control to telehealth services, the division of health sciences touches every corner of public and personal well-being. Graduates of health sciences programs work as:
- Clinical Practitioners
- Public Health Experts
- Health Policy Advisors
- Biomedical Researchers
- Health Educators
- Pharmacists
These professionals contribute to healthcare not only through clinical services but also by shaping health policies, conducting life-saving research, and improving access to care.
Emphasis on Community Engagement
Community engagement is another cornerstone of the division of health sciences. Institutions promote fieldwork and service-learning opportunities that allow students to serve underserved populations while applying their knowledge in real-world settings. These efforts often involve:
- Free medical camps
- Health awareness drives
- Mobile clinics in remote regions
- Partnerships with NGOs and local governments
This ensures that students understand the real challenges faced by diverse communities and are better prepared to respond with empathy and skill.
Technological Integration in Health Sciences
Technology is revolutionizing how education and patient care are delivered. The division of health sciences has rapidly adopted innovations such as:
- Virtual Simulation Labs: For safe, controlled learning experiences
- Electronic Health Records (EHR): For streamlined data management
- AI-Powered Diagnostic Tools: Enhancing accuracy and speed
- Telemedicine Platforms: Increasing healthcare access for remote areas
These tools not only improve the quality of education but also make healthcare delivery more efficient and effective.
Global Health and International Collaboration
Global health is a vital focus area for many health sciences divisions. Collaborating with international health organizations enables institutions to tackle widespread health issues like pandemics, maternal health disparities, and non-communicable diseases.
These collaborations often include:
- Cross-border research initiatives
- Student and faculty exchange programs
- Joint degrees and dual certification
- Participation in global health summits
Through these partnerships, the division of health education helps shape policies and strategies on a global scale.
Career Opportunities for Graduates
Graduates from the division of health sciences enjoy diverse career options in both clinical and non-clinical roles. Here are some common career paths:
- Clinical Medicine: Doctors, surgeons, anesthesiologists
- Nursing & Midwifery: Hospital-based or community-based practice
- Public Health: Epidemiologists, health policy planners
- Pharmacy: Clinical pharmacists, drug safety officers
- Health Technology: Health informaticians, telehealth coordinators
- Research: Biomedical researchers, clinical trial specialists
The variety of opportunities ensures that every student can find a pathway aligned with their passion and skillset.
Addressing Healthcare Disparities
Health equity is central to the mission of the division of health education. Through education, policy advocacy, and community involvement, these institutions work to reduce healthcare disparities among marginalized populations. Initiatives focus on:
- Increasing access to care in rural and underserved areas
- Promoting culturally competent care
- Supporting minority representation in healthcare professions
- Researching social determinants of health
This commitment to equity ensures that healthcare systems become more inclusive and responsive.
Lifelong Learning and Continuing Education
The healthcare industry evolves rapidly. That’s why the division of health education supports lifelong learning through continuing education programs, certifications, and advanced degrees. Professionals are encouraged to stay updated on:
- New treatment protocols
- Regulatory compliance
- Emerging health threats
- Ethical standards
These programs help healthcare workers maintain their licensure, expand their skills, and remain competitive in the field.
Accreditation and Quality Assurance
Quality assurance in the division of health sciences is maintained through rigorous accreditation processes. These ensure that academic programs meet national and international educational standards. Accreditation bodies assess:
- Curriculum quality
- Faculty qualifications
- Research output
- Clinical affiliations
- Student support services
Such standards build public trust and guarantee that graduates are well-prepared to enter the workforce.
Student Support and Mentorship
A well-structured division of health education prioritizes student success through mentorship, academic advising, and career counseling. Support services may include:
- Peer mentoring
- Skills development workshops
- Resume and interview coaching
- Research opportunities with faculty
These resources foster a strong academic foundation and professional readiness.
Environmental Health and Sustainability
With growing awareness of climate-related health risks, many health sciences divisions are incorporating sustainability into their curricula. Topics include:
- Air and water quality monitoring
- Waste management in hospitals
- Sustainable healthcare infrastructure
- Climate change and disease trends
This prepares future health leaders to respond to environmental health challenges with knowledge and initiative.
Enhancing Health Literacy
Health literacy plays a significant role in patient outcomes. The division of health education works to promote health literacy through:
- Patient education tools
- Community health worker training
- Accessible healthcare communication strategies
- Bilingual and culturally relevant resources
Improved health literacy empowers individuals to make informed decisions and engage effectively with healthcare services.
Global Trends Shaping Health Sciences
Emerging global trends influence how the division of health education evolves. Some key trends include:
- Rise of personalized medicine
- Greater integration of mental health into primary care
- Focus on preventative rather than reactive care
- Data-driven health decision-making
- Shift towards community-based healthcare delivery
Staying ahead of these trends is crucial for academic institutions to maintain relevance and impact.
Conclusion
The division of health sciences remains an indispensable pillar of modern healthcare. Through interdisciplinary education, cutting-edge research, and global collaboration, it equips students and professionals to meet the world’s most pressing health challenges. Whether in public health, clinical medicine, or healthcare innovation, the division drives excellence, equity, and impact across the healthcare continuum.
FAQs
What is the division of health sciences?
The division of health sciences is an academic and research branch within institutions that encompasses various disciplines like medicine, public health, nursing, pharmacy, and allied health to improve healthcare outcomes.
Which careers can one pursue with a health sciences degree?
Graduates can work as doctors, nurses, public health officials, pharmacists, researchers, or healthcare technology specialists, depending on their area of specialization.
How does health sciences education differ from traditional medical education?
Health sciences education is broader and includes various fields like public health, allied health, and informatics, while traditional medical education focuses primarily on physician training.
Is the division of health sciences involved in research?
Yes, it plays a major role in healthcare research, focusing on innovations in diagnostics, treatment, health policy, and disease prevention.
What skills are important for success in health sciences?
Key skills include communication, problem-solving, teamwork, critical thinking, and adaptability, as well as technical proficiency relevant to specific disciplines.
Can health sciences graduates work internationally?
Absolutely. Many health sciences degrees are globally recognized, and professionals can work with international NGOs, research institutes, and healthcare organizations around the world.
HEALTH
Sonrava Health: A Modern Approach to Community Dental Care

Sonrava Health is reshaping how communities experience dental care across the United States. At a time when access, affordability, and patient comfort matter more than ever, this dental support organization focuses on creating a reliable and efficient care network. Instead of operating as a traditional single clinic, Sonrava Health supports multiple dental brands and offices, helping them deliver consistent and high-quality services. With a strong emphasis on patient-centered dentistry, innovation, and operational excellence, the company continues to grow its footprint in modern healthcare.
What Is Sonrava Health?
Sonrava Health is a dental support organization that partners with affiliated dental practices to provide administrative, operational, and strategic support. By handling non-clinical responsibilities such as billing, staffing coordination, marketing, and compliance, the organization allows dentists to focus fully on patient care. This model improves efficiency while maintaining clinical independence at the practice level.
The company supports thousands of dental professionals across multiple states, making it one of the significant players in the dental services industry. Its approach blends business expertise with healthcare management, ensuring that patients receive consistent service standards. Through centralized systems and advanced technology, Sonrava Health strengthens both patient outcomes and practice performance.
A Network of Trusted Dental Brands
One of the key strengths of Sonrava Health lies in its network of affiliated dental brands. The organization supports well-known names such as Western Dental & Orthodontics and Brident Dental & Orthodontics, which serve diverse communities. These brands offer general dentistry, orthodontics, oral surgery, pediatric dentistry, and cosmetic procedures under one roof.
By working with established dental providers, Sonrava Health ensures patients have access to comprehensive oral healthcare services in convenient locations. The network model allows standardized quality control while respecting the clinical judgment of licensed dentists. This balance of structure and flexibility supports long-term growth and patient satisfaction.
Focus on Accessible and Affordable Care
Access to affordable dental care remains a major concern in many communities. Sonrava Health addresses this challenge by supporting practices that accept a variety of insurance plans, including Medicaid and managed care programs. This helps families, children, and underserved populations receive essential oral healthcare without financial strain.
The organization also encourages flexible payment options and transparent pricing models. By streamlining administrative processes and improving operational efficiency, affiliated clinics can reduce overhead costs and pass savings to patients. This commitment to affordability strengthens community trust and expands care access.
Commitment to Quality and Technology
Modern dentistry relies heavily on innovation, and Sonrava Health integrates advanced dental technology across its supported practices. Digital imaging, electronic health records, and modern diagnostic tools enhance accuracy and treatment planning. These systems improve workflow efficiency while ensuring a safer and more comfortable patient experience.
Quality assurance is another core focus. The organization provides compliance guidance, training resources, and operational oversight to maintain high standards. Through continuous improvement strategies, affiliated clinics remain aligned with evolving healthcare regulations and patient care best practices.
Career Opportunities and Professional Growth
Sonrava Health also plays an important role in supporting dental professionals. Dentists, hygienists, assistants, and administrative staff benefit from structured career pathways, training programs, and leadership opportunities. This environment encourages long-term professional growth within a stable healthcare network.
By offering operational support and collaborative systems, the organization reduces the business burden on clinicians. This allows dental professionals to concentrate on delivering high-quality care while advancing their careers. A strong workforce directly contributes to better patient outcomes and consistent service standards.
Community Impact and Long-Term Vision
Beyond business operations, Sonrava Health aims to improve overall oral health awareness in the communities it serves. Preventive dentistry, early diagnosis, and patient education are central to its mission. By encouraging routine checkups and proactive treatment, affiliated practices help reduce long-term dental complications.
The organization’s long-term vision focuses on sustainable growth, innovation in dental services, and expanded access to underserved populations. As the dental industry continues to evolve, Sonrava Health positions itself as a forward-thinking healthcare partner that blends operational strength with compassionate patient care.
Conclusion
Sonrava Health represents a modern model of dental support that combines operational expertise with patient-centered values. By partnering with trusted dental brands, integrating advanced technology, and prioritizing affordability, the organization strengthens community access to quality oral healthcare. Its commitment to professional development and compliance ensures stability within a rapidly changing healthcare landscape. For patients seeking reliable dental services and for professionals pursuing structured career growth, Sonrava Health stands as a trusted and forward-looking name in the dental services industry.
FAQs
What is Sonrava Health?
Sonrava Health is a dental support organization that provides administrative and operational services to affiliated dental practices.
Does Sonrava Health provide direct dental treatment?
No, it supports dental clinics and brands, while licensed dentists deliver the actual clinical care.
What services are offered within its network?
Affiliated practices offer general dentistry, orthodontics, pediatric care, cosmetic treatments, and oral surgery.
Is Sonrava Health focused on affordable care?
Yes, many supported clinics accept various insurance plans and provide flexible payment options.
Where does Sonrava Health operate?
It operates across multiple U.S. states through its network of affiliated dental brands.
HEALTH
Braven Health Smart Card — Benefits, Usage & Key Details
HEALTH
Tina Jones HEENT Shadow Health Assessment – Steps, Findings & Tips

The Tina Jones HEENT Shadow Health assessment is one of the most important modules in the Shadow Health Digital Clinical Experience (DCE) for nursing students. It focuses on the Head, Eyes, Ears, Nose, and Throat (HEENT) examination and helps learners develop hands-on clinical reasoning, data collection, and patient interaction skills through a virtual environment.
In this assessment, students interact with a simulated patient, Tina Jones, to gather both subjective and objective data. This experience is designed to prepare students for real-life patient encounters by emphasizing communication, observation, and assessment skills.
What Is the Tina Jones HEENT Shadow Health Assessment?
The Tina Jones HEENT Shadow Health module is an interactive simulation where you perform a focused assessment of the patient’s head, eyes, ears, nose, and throat. You collect health history, perform examinations, identify abnormalities, and document findings—just as you would in a real clinical setting.
Tina Jones is a 28-year-old patient presenting with mild nasal congestion and throat discomfort, giving students an opportunity to evaluate both normal and mild abnormal findings in a controlled digital environment.
Objectives of the Assessment
The main goal of the Tina Jones HEENT Shadow Health simulation is to enhance clinical competence and patient-centered communication. By completing this activity, students learn to:
-
Conduct a thorough health history relevant to HEENT.
-
Use correct examination techniques to assess each component.
-
Identify and interpret normal versus abnormal findings.
-
Document data accurately and provide education based on findings.
Through this process, students build confidence and learn how to connect theoretical knowledge with real-world application.
Step-by-Step Guide to Completing the HEENT Assessment
1. Establish Communication and Gather Health History
Start your assessment by greeting Tina Jones politely and introducing yourself. Establishing rapport helps her feel comfortable and encourages open communication. Ask open-ended questions such as:
-
“Can you tell me about any discomfort or issues you’re experiencing with your eyes, ears, nose, or throat?”
-
“When did your symptoms start?”
-
“Do you have any allergies or past medical conditions related to the head or neck?”
Tina often reports mild nasal congestion and occasional sore throat, symptoms consistent with seasonal allergies or mild upper respiratory irritation. Always document her responses carefully as subjective data.
2. Head and Face Examination
Inspect the head and face for symmetry, contour, and signs of trauma or deformity. Ask Tina if she has experienced headaches, dizziness, or facial tenderness. Palpate the frontal and maxillary sinuses to check for tenderness.
Typical findings during the Tina Jones HEENT Shadow Health assessment include:
-
Head: Normocephalic, no tenderness, symmetrical.
-
Face: No lesions, swelling, or drooping.
-
Sinuses: No tenderness to palpation.
Document these observations as objective data since they indicate normal health.
3. Eye Examination
The eye exam focuses on evaluating visual health and neurological function. Start by assessing visual acuity and observing external structures like the sclera, conjunctiva, and pupils.
Use the PERRLA method (Pupils Equal, Round, Reactive to Light and Accommodation) to assess pupil response. Tina’s typical findings are:
-
Pupils equal and reactive to light.
-
Sclera white, conjunctiva pink and clear.
-
No visual disturbances or eye pain.
| Eye Assessment Components | Expected Normal Findings |
|---|---|
| Visual acuity | Normal vision, no blurriness |
| Conjunctiva and sclera | Pink conjunctiva, white sclera |
| Pupil reaction (PERRLA) | Equal and responsive |
| Eye movements | Smooth and coordinated |
These results demonstrate a healthy ocular system and intact cranial nerves.
4. Ear Assessment
Inspect and palpate the external ear structures for lesions, redness, or discharge. Ask Tina about any hearing loss, tinnitus, or ear pain. Perform a quick whisper test to assess hearing acuity.
In most Tina Jones HEENT Shadow Health cases, findings are:
-
External ears symmetrical and intact.
-
No pain or discharge.
-
Hearing intact bilaterally.
If any earwax buildup or discomfort is present, document it and educate the patient about safe ear hygiene practices.
5. Nose and Sinus Examination
Next, assess Tina’s nasal structure and mucosa. Use a penlight to inspect inside the nostrils for redness, swelling, or discharge. Ask about nasal congestion, drainage, or allergies.
You may find mild nasal congestion and clear discharge, which are common in allergy-related cases. Palpate the sinuses for tenderness. Tina usually denies sinus pain, indicating no infection.
| Nasal Assessment Area | Common Finding | Interpretation |
|---|---|---|
| Nasal mucosa | Pink, moist | Healthy tissue |
| Septum | Midline, intact | Normal alignment |
| Sinuses | No tenderness | No sinus infection |
6. Mouth and Throat Examination
Inspect the lips, teeth, gums, tongue, tonsils, and pharynx. Ask if Tina has any difficulty swallowing or sore throat.
Her typical findings include slightly red pharynx, tonsils 1+, and moist oral mucosa. This mild redness usually indicates postnasal drip rather than infection.
Educate Tina about increasing water intake, using saline gargles, and avoiding irritants like smoke or strong fragrances.
Interpreting Common Findings in the Tina Jones HEENT Assessment
| Area | Typical Finding | Possible Interpretation |
|---|---|---|
| Head | Symmetrical, normocephalic | Normal anatomy |
| Eyes | PERRLA, conjunctiva clear | No visual disorder |
| Ears | Hearing intact | No hearing loss |
| Nose | Mild congestion | Seasonal allergies |
| Throat | Slight redness | Postnasal drip |
Understanding these findings helps you differentiate between benign conditions and those requiring further evaluation.
Documentation and Patient Education
Accurate documentation is essential in the Tina Jones HEENT Shadow Health module. Record both subjective data (patient-reported symptoms) and objective data (observed findings). Use correct medical terminology and avoid assumptions.
For patient education, advise Tina to:
-
Stay hydrated to reduce throat irritation.
-
Use a humidifier to ease congestion.
-
Avoid allergens and keep the environment clean.
-
Seek medical care if symptoms persist or worsen.
Document all teaching points and the patient’s understanding in your charting section.
Tips for Success in the Shadow Health HEENT Assessment
To perform well in the Tina Jones HEENT Shadow Health simulation, preparation and attention to detail are key. Review the anatomy and physiology of the head and neck region before starting. Take your time to ask all relevant questions—completeness affects your Digital Clinical Experience (DCE) score.
When documenting, make sure your statements are concise, objective, and free from judgmental language. Use the simulation’s checklists to verify you haven’t missed any component of the assessment.
Summary
The Tina Jones HEENT Shadow Health assessment is an excellent opportunity for nursing students to strengthen their clinical judgment, data collection, and communication skills. By understanding how to conduct a thorough head, eyes, ears, nose, and throat exam, learners gain confidence that translates to real-world patient care.
Mastering this module requires good preparation, active listening, and clear documentation. When completed effectively, it enhances your clinical readiness and overall nursing competence.
FAQs
1. How long does the Tina Jones HEENT Shadow Health assessment take to complete?
Typically, it takes between 45 to 60 minutes depending on your familiarity with HEENT systems.
2. Can I repeat the assessment to improve my score?
Yes, most nursing instructors allow multiple attempts to help you improve your DCE performance.
3. Are Tina Jones’s symptoms always the same?
They may vary slightly based on your responses and the simulation version, but the main findings remain consistent.
4. Do I need to use specific medical terminology in documentation?
Yes, using professional nursing and medical terminology improves clarity and grading accuracy.
5. What percentage of my course grade is this assessment worth?
This depends on your nursing program, but it typically contributes around 5–10% of your clinical evaluation score.
dow health
-
 GENERAL7 months ago
GENERAL7 months agoRobert Hubbell Wikipedia: What’s His 2025 Biography Guide?
-

 EDUCATION9 months ago
EDUCATION9 months agoJay Kuo Substack: Unpacking the Voice of Legal Insight
-

 GENERAL9 months ago
GENERAL9 months agoDream Cake: A Decadent Delight Worth Savoring
-

 GENERAL9 months ago
GENERAL9 months agoChris Hedges Substack: A Voice of Dissent in the Digital Age
-

 ENTERTAINMENT9 months ago
ENTERTAINMENT9 months agoTyler the Creator Dad Truth
-
 TECHNOLOGY9 months ago
TECHNOLOGY9 months agoHow to Cancel Substack Subscription
-

 EDUCATION9 months ago
EDUCATION9 months agoEconomic Blackout Results: The Financial Domino Effect
-
 GENERAL9 months ago
GENERAL9 months agoMax Azzarello Substack: Inside the Mind of a Radical Truth-Seeker

